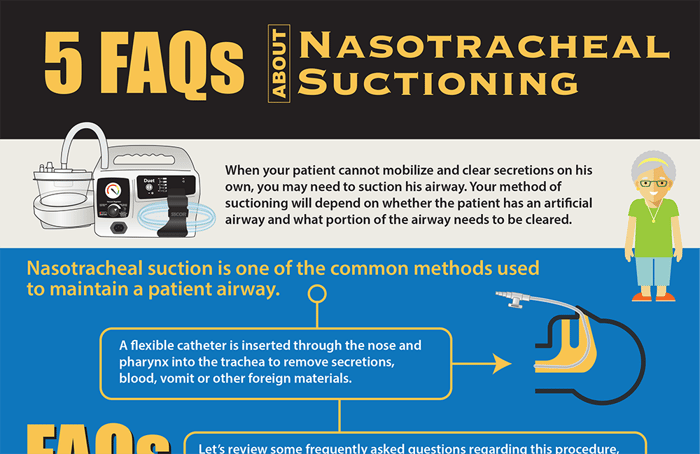
When your patient cannot mobilize and clear secretions independently, you may need to suction their airway. Your suctioning method will depend on whether the patient has an artificial airway and what portion of the airway needs to be cleared.
Nasotracheal suction is one of the common methods used to maintain a patent airway. A flexible catheter is inserted through the nose and pharynx into the trachea to remove secretions, blood, vomit, or other foreign materials.
Let’s review some frequently asked questions regarding this procedure, following the American Association for Respiratory Care’s Clinical Practice Guidelines for Nasotracheal Suctioning.
1. How do I know that my patient needs to be suctioned?
The presence of visible or audible secretions is the clearest indication. You may also notice your patient working harder to breathe or acting restless and uncomfortable. On auscultation, you may hear coarse or diminished breath sounds. Your patient may show changes in respiratory rate, heart rate, oxygen saturation, skin color, and perfusion. Blood gases may show difficulty with oxygenation and ventilation, and chest X-rays may reveal areas of atelectasis or consolidation.
2. Are there any contraindications to suctioning my patient?
Epiglottitis or croup are considered absolute contraindications to nasotracheal suctioning. Other situations, while not absolutely contraindicated, that need to be taken into consideration include head or neck injury, laryngospasm and bronchospasm, occluded nasal passages, and bleeding disorders.
3. What complications can occur as a result?
The most common complication is physical trauma to the nose and pharynx. Gagging or vomiting can occur. Changes in heart rate, rhythm, and blood pressure may be seen. Patients may become hypoxic. There is a risk of infection. Atelectasis, pneumothorax, and increased intracranial pressure may also result.
4. What materials do I need to perform nasotracheal suction?
You will need either an in-wall or portable suction to act as your vacuum source, as well as a regulator for adjusting suction strength. In addition, you’ll need:
- A collection vessel, suction tubing, and a flexible, multi-eyed suction catheter.
- Sterile gloves should be worn during the procedure.
- Water-based lubricant or normal saline can be used to lubricate the tip of the catheter, making insertion easier.
- A cup of sterile water can be used to clean the catheter between passes.
Consider using a local anesthetic or a nasopharyngeal airway when frequent suctioning will be needed. Always keep a bag and mask nearby.
5. How should I monitor my patient during and after the procedure?
Vital signs should be watched closely before and after suctioning. Pay attention to breath sounds, noting if an improvement occurs when suction is complete. Note the amount of secretions, as well as any changes in color or consistency, and assess for signs of mucosal trauma or blood after suctioning.
If your patient has a pulse oximeter or intracranial pressure monitor in place, watch for any changes during and after the procedure. Assess your patient’s pain level. Watch for adverse reactions such as bradycardia or laryngospasm.
Though nasotracheal suction may be seen as a routine procedure, it is not without risk. Taking some time to review the process and ensure that you are using best practices is the responsibility of every great nurse.
Editor's Note: This blog was originally published in May 2024. It has been re-published with additional up to date content.
















