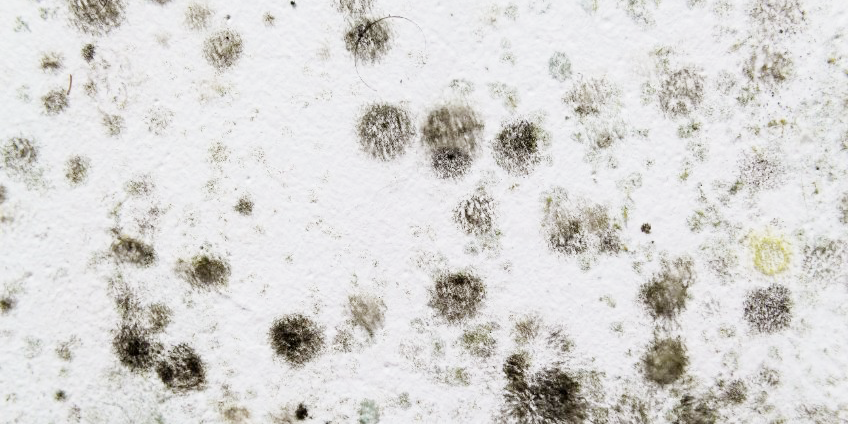
Mold can present dangers for individuals in their homes, office spaces and many other indoor and outdoor environments. Notably, as a fungal growth that forms on damp and decaying organic matter and grows during all seasons of the year, mold can cause a range of respiratory emergencies if its spores are inhaled.
To prevent the development of mold infections and other airway concerns, it’s critical that EMS providers know what dangers to look for and the airway management techniques to employ when treating patients who have been exposed to mold. We’ve put together some information to help providers understand respiratory symptoms caused by mold, and their impact on individuals with various respiratory concerns.
Occurrence and causes
Mold is sneaky and invasive — it can form and grow from even the slightest exposure to outdoor elements. It can enter the home through open doors, windows, vents or heating and air conditioning systems. Mold in the air outside can also be tracked indoors on clothing, shoes, bags and even pets.
The formation and growth of mold varies in indoor and outdoor environments. In indoor environments, molds rely on moisture from building materials as a carbon source to grow and spread. Office buildings are common sources of mold growth, due to their moderate temperatures and available building materials as nutrient sources. Homes are more likely to grow mold after a major flood or related weather event, and the mold may last for weeks or longer if not treated properly. In outdoor environments, molds use plants and decaying organic matter, such as fallen leaves and branches, as nutritional sources.
Respiratory considerations and emergencies
There are various respiratory factors to consider when treating patients who have been exposed to mold, which can lead to many health issues, including stuffy nose, sore throat, coughing or wheezing, burning eyes and skin rashes. But special attention must be given to individuals with preexisting conditions. For example, people with chronic lung disease may develop infections in their lungs from mold exposure, and immunocompromised individuals can develop invasive mold infections days or weeks after initial exposure to fungi in their environment. Some risk factors for developing mold infections include:
- If an individual has had a transplant, especially hematopoietic stem cell transplants
- Cancer, particularly hematologic cancers like leukemia and lymphoma
- Taking medications that weaken the immune system, such as corticosteroids and biologics
- Undergoing chemotherapy or other cancer treatments
Mold is a common asthma trigger for many people, and individuals with asthma should do everything they can to avoid staying in a moldy home or being inside the home while it’s being cleaned. In addition to inhaling medications, identifying and avoiding asthma triggers can help individuals with asthma mitigate risks related to mold exposure and infection. In the worst-case scenarios, asthma triggers can lead to respiratory failure. Between 3-5% of adults hospitalized for acute asthma develop respiratory failure requiring mechanical ventilation. Common symptoms of respiratory failure include:
- Severely altered mental state
- Labored breathing and use of accessory muscles
- Inability to speak
- Severe cyanosis (bluish skin resulting from a lack of oxygen)
- No breathing sounds
- Decreased O2 saturation even with O2 or other interventions
- A heartbeat consistently higher than 130 beats per minute (for an adult)
Airway management and suctioning
When treating an asthmatic patient, the first line of defense against an asthma attack should always be a rescue inhaler, followed by medication if the inhaler is unsuccessful, and then mask ventilation.
EMS providers must be aware that inflammation from asthma can compromise the airway, making intubation extremely difficult and dangerous. For this reason, responders should only intubate after medication has failed or the patient exhibits severe oxygen deficiency.
The steps EMS providers should follow to perform ventilation as safely and efficiently as possible include:
- Practicing thorough hygiene before, during and after ventilation
- Explaining the procedure fully to the patient and being sure to receive consent before proceeding
- Sedating the patient so they experience no pain or anxiety during the procedure
- Suctioning the patient with the right-size catheter prior to ventilation
- Preparing the ventilator with age and size appropriate settings for volume, breaths per minute and positive and expiratory pressure
- Keeping the patient’s caregiver informed of the treatment plan every step of the way
Remaining prepared
No matter what environment someone is in, there will always be some mold around, but knowing what exposure symptoms to look for will help providers better educate patients about the health risks of mold in homes and other settings. You and your team should remain prepared by becoming knowledgeable about the signs and symptoms of mold infections and other respiratory emergencies, as well as practice various suctioning and ventilation techniques for treating patients during airway emergencies.
Read this article on intubation and ventilation of the asthmatic patient to learn more about emergency ventilation and airway management.













